gut flora
now browsing by tag
Eat It Dirty
Two words: gut flora.
A pair of articles that appeared recently in the New York Times provide some good leads on why our reactions to food may be changing, why people eating the same diet today may be reacting to it differently than people did 40 years ago.
 First, Michael Pollan’s latest piece in the New York Times Magazine, Some of My Best Friends Are Germs, dives into the hidden world inside us and on us: the 100’s of trillions of bacteria that inhabit our gut, our skin and everywhere in between.
First, Michael Pollan’s latest piece in the New York Times Magazine, Some of My Best Friends Are Germs, dives into the hidden world inside us and on us: the 100’s of trillions of bacteria that inhabit our gut, our skin and everywhere in between.
I won’t do it justice, but I’ll give it a shot anyway: our bodies are chock full of microbes. In fact, for every one human cell in your body, there are about 10 non-human microbes. Many of these microbes have co-evolved with us, and play important roles in our health.
Small example:
We’ve known for a few years that obese mice transplanted with the intestinal community of lean mice lose weight and vice versa. (We don’t know why.) A similar experiment was performed recently on humans by researchers in the Netherlands: when the contents of a lean donor’s microbiota were transferred to the guts of male patients with metabolic syndrome, the researchers found striking improvements in the recipients’ sensitivity to insulin, an important marker for metabolic health. Somehow, the gut microbes were influencing the patients’ metabolisms.
And also:
Most of the microbes that make up a baby’s gut community are acquired during birth — a microbially rich and messy process that exposes the baby to a whole suite of maternal microbes. Babies born by Caesarean, however, a comparatively sterile procedure, do not acquire their mother’s vaginal and intestinal microbes at birth. Their initial gut communities more closely resemble that of their mother’s (and father’s) skin, which is less than ideal and may account for higher rates of allergy, asthma and autoimmune problems in C-section babies: not having been seeded with the optimal assortment of microbes at birth, their immune systems may fail to develop properly.
Much research has gone into one microbe in particular, Helicobacter pyolori (H. Pylori):
The microbe engages with the immune system, quieting the inflammatory response in ways that serve its own interests — to be left in peace — as well as our own. This calming effect on the immune system may explain why populations that still harbor H. pylori are less prone to allergy and asthma. Blaser’s lab has also found evidence that H. pylori plays an important role in human metabolism by regulating levels of the appetite hormone ghrelin. “When the stomach is empty, it produces a lot of ghrelin, the chemical signal to the brain to eat,” Blaser says. “Then, when it has had enough, the stomach shuts down ghrelin production, and the host feels satiated.” He says the disappearance of H. pylori may be contributing to obesity by muting these signals.
And H. pylori is nearly extinct in the Western gut.
So the various organisms that live in us and on us help us digest our food, help teach our immune system which microbes are friend and which are foe and perform other key functions in helping us live the way we evolved to.
So, what’s changed?
Well, there’s the obvious: “Children in the West receive, on average, between 10 and 20 courses of antibiotics before they turn 18,” according to Pollan. Each of those treatments carpet bombs the gut, ridding it indiscriminately of both beneficial and dangerous colonies of microbes. Some colonies bounce back, others don’t.
Of course, prescribed antibiotics taken directly are only part of the problem: all non-organically raised farm animals in the United States receive low doses of antibiotics their whole lives (see this Michael Pollan interview for why that is), so if you’ve eaten meat, you’ve been taking low doses of antibiotics every day of your life, further stressing your internal ecosystem.
But Pollan brings up a whole other set of influencers: the care and feeding of your microcolonies. The bacteria in your body need particular nutrients to thrive, as well. This starts early:
For years, nutrition scientists were confounded by the presence in human breast milk of certain complex carbohydrates, called oligosaccharides, which the human infant lacks the enzymes necessary to digest. Evolutionary theory argues that every component of mother’s milk should have some value to the developing baby or natural selection would have long ago discarded it as a waste of the mother’s precious resources.
It turns out the oligosaccharides are there to nourish not the baby but one particular gut bacterium called Bifidobacterium infantis, which is uniquely well-suited to break down and make use of the specific oligosaccharides present in mother’s milk. When all goes well, the bifidobacteria proliferate and dominate, helping to keep the infant healthy by crowding out less savory microbial characters before they can become established and, perhaps most important, by nurturing the integrity of the epithelium — the lining of the intestines, which plays a critical role in protecting us from infection and inflammation.
Which brings up the second article, Breeding the Nutrition Out of Our Food, which shows how the foods that we eat, even the whole food produce, has become gradually less nutritious over time, as we’ve bred it for flavor and sweetness.
Phytonutrients are a set of compounds produced in plants that have generally positive health effects for humans: they’ve been shown to reduce the risk of cancer, cardiovascular disease, diabetes and dementia, to name a few.
And they’ve been disappearing from our foods.
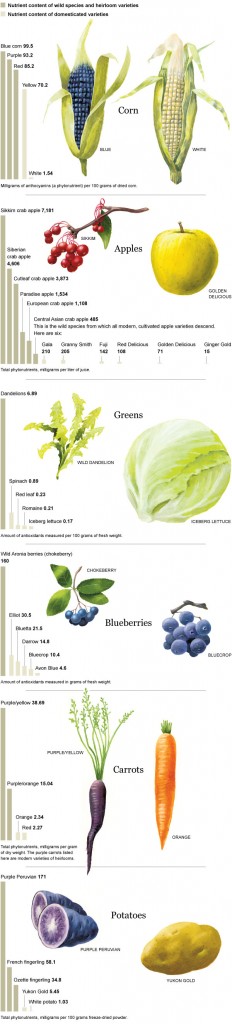
While I’d love to use this data to slap my GMO-loving friends in the face, the truth is it goes back much further than the 20th century. Since the beginning of agriculture, we’ve been selectively breeding our produce for sweetness and taste over the presence of phytonutrients (which often come with bitterness). Wild dandelions, for example, have seven times more phytonutrients than spinach. Purple potates have 28 times the cancer-fighting anthocyanin than russet potatoes. The ancestors of apples have a 100 times the phytonutrient content as most modern apples.
But we’ve certainly accelerated the trend: the sweet, juicy corn that we eat today simply didn’t exist a mere 200 years ago. Iceberg lettuce has about 1/5th the phytonutrients as spinach. The attractive orange variety of carrot that is the only kind available in most supermarkets has 1/7th the phytonutrients as their purple/orange cousins and less than 1/15th as much as their purple/yellow cousins.
So the food that we feed ourselves has been changing, and the food that we feed the microbial ecosystem that helps us digest our food has changed. Are you surprised that our reactions to food have changed?
So what are we supposed to do with all this? Here’s my take-away:
- Unless you’re a doctor scrubbing in, ditch the anti-bacterial soap and the bleach on everything. Let it grow.
- Consider giving your natural immune system a chance to deal with infections before resorting to antibiotics.
- Look for heirloom and wild varieties of fruits and vegetables.
- Eat root vegetables with the skin on: the skin is where most of the nutrients and microbiota are.
- Seek out fermented foods: kombucha, kimchi and raw-milk cheese, to name a few. They’re alive!
And there was one more passage from Pollan’s article that stuck out for me:
The data helped demonstrate that the microbial communities of couples sharing a house are similar, suggesting the importance of the environment in shaping an individual’s microbiome. Knight also found that the presence of a family dog tended to blend everyone’s skin communities, probably via licking and petting.
So, just as vaginal birth can help pass microbiota from mother to child, establishing a healthy ecosystem, the family dog licking everyone’s hands helps spread the beneficial microbiota from person to person within a household.
Don’t have a dog? Kiss your baby!